Gastroenterology and Hepatology overview
Gastroenterology and Hepatology is the branch of medicine focused on the digestive system and its disorders. This includes prevention, diagnosis and treatment of conditions involving the oesophagus, stomach, small intestine, colon, pancreas, liver and gall bladder. These conditions range from being seen frequently to others that are rare disorders. The Oxford Virtual Hospital has specifically chosen specialists with extensive experience to enable us to cater for your specific needs. Personalised medicine is at the heart of our treatment goals, ensuring that you receive the best possible care.
Diagnosing and treating these disorders is very important as suffering with abdominal symptoms can have a significant effect on your quality life. Gastrointestinal symptoms can be embarrassing as well as disabling. Finding out what the problem is and actively taking steps to manage this is very likely to improve your social, emotional and occupational well-being.

Gastroenterologists and Hepatologists perform a number of diagnostic and therapeutic procedures including gastroscopy, colonoscopy, liver biopsy and fibroscan.
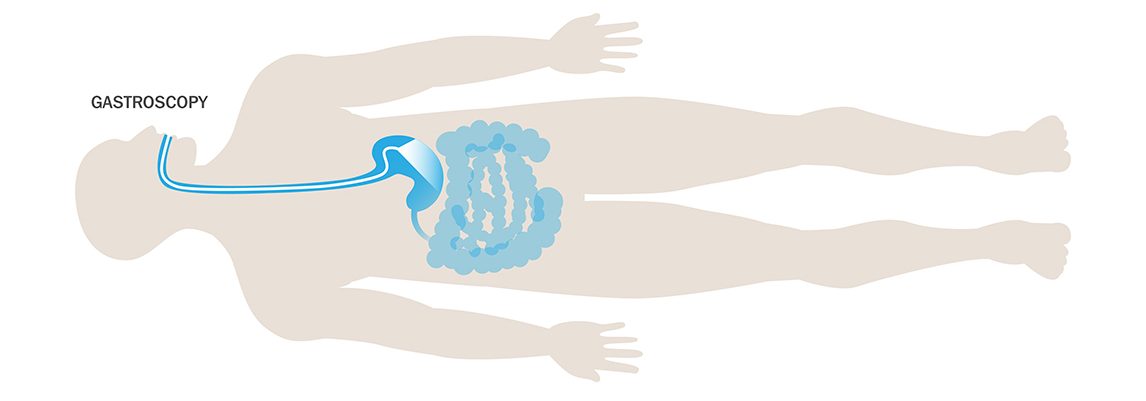
Gastroscopy
A gastroscopy (examination of the stomach) can help to confirm or rule out the presence of medical conditions such as gastritis, peptic ulcers, or coeliac disease. In this procedure, an instrument called a gastroscope is used to look at the inside of the oesophagus (food pipe), the stomach and the first part of the small intestine.
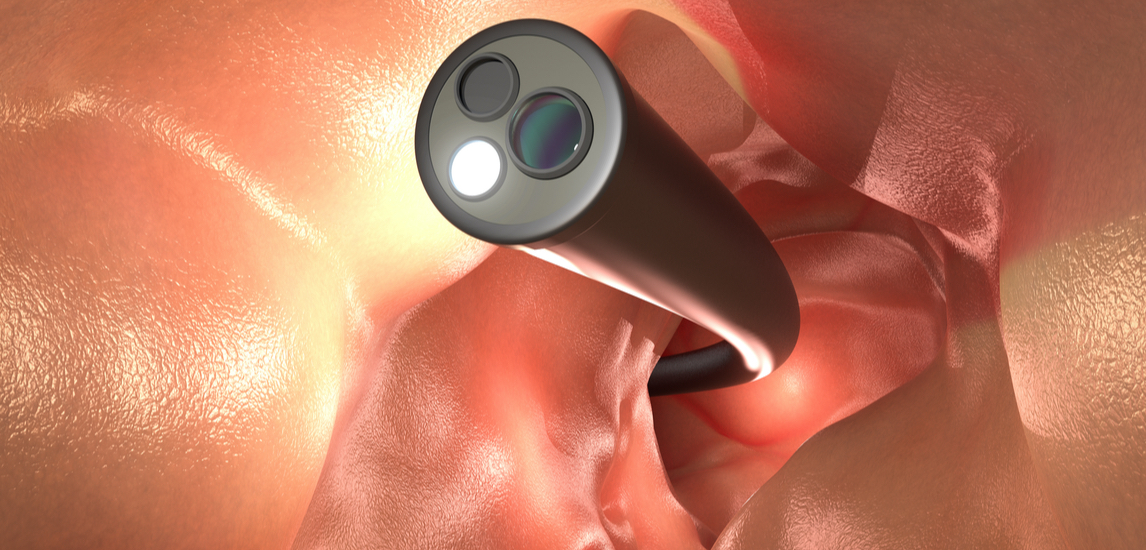
Colonoscopy
A colonoscopy is a test to check inside your bowels with the aim of finding out what is causing your symptoms and/or to look for any abnormal growths. A long, thin, flexible tube with a small camera inside it is passed into your bottom. You will be given a laxative prior to this procedure to ensure that your bowels are empty for the test.
FibroScan®
FibroScan® is a safe, painless, non-invasive test to look for evidence of liver scarring. It is a form of transient elastography whereby a probe is placed against the skin overlying the liver on the right side. A gentle pulse is emitted and the speed that the pulse travels through the liver is measured using ultrasound. An average of 10 readings is taken as the liver stiffness measurement (in kiloPascals, kPa), which correlates with the degree of fibrosis (scarring) in the liver.
Liver stiffness measurement is helpful in determining the severity of many chronic liver diseases and will commonly form part of the diagnostic work-up. In addition, it can be helpful to test the liver stiffness in patients with cirrhosis of the liver to determine the risk of certain complications including the presence of oesophageal varices.
Many FibroScan® machines have a capability called CAP (controlled attenuation parameter). This provides a measure of liver fat which can provide helpful additional information.
Liver biopsy
Liver biopsy is the process of obtaining a small amount of liver tissue to look at under the microscope. It is used to help diagnose liver diseases where the cause is unclear from non-invasive tests, where more than one cause of liver disease may be at play, or to determine the severity of liver disease if non-invasive tests do not provide a clear answer. Usually the sample is of the liver tissue (“parenchyma”), but sometime the target is a liver lesion or lump. Many clinical research trials also make use of liver biopsy as the “gold standard” test.
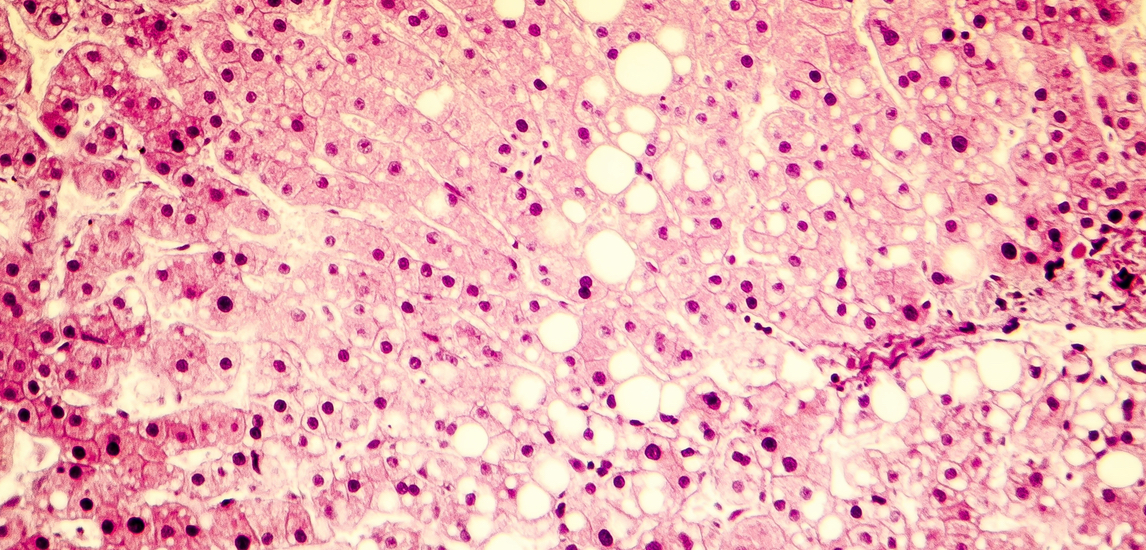
Liver biopsy is usually carried out as a daycase procedure. Most are performed percutaneously, using a needle that is passed through the skin overlying the liver between the ribs on the right side using ultrasound guidance to obtain a fine core of liver tissue. The procedure requires local anaesthetic, takes just a few minutes and is usually very well tolerated. Afterwards, the patient is required to lie down for 4-6 hours for observation to ensure they are safe, recover well and to give painkillers if required. Approximately 1/3 of patients require some simple painkillers, 1 in 30 have more severe pain requiring stronger painkillers, while 1:300 to 1:500 have a more severe complication requiring hospital treatment such as interventional radiology, surgery or blood transfusion. In selected patients, a transjugular route is recommended. This is where the liver is accessed through a vein in the neck in the interventional radiology department. This route is used where the blood clotting is insufficient, where there is ascites (fluid) in the abdomen, or where the doctors need to assess the pressure in the blood vessels in the liver.
The liver biopsy is processed and analysed by histopathology specialists, so take a few days for the result to be available. Special further tests on the tissue sample may take longer.


